RQO Committee Overview
The Research, Quality and Outcomes (RQO) Committee mission is to carry out charges set forth by the NSGC Board of Directors centered around demonstrating the value of genetic counseling and generating the data for evidence based practice. The RQO committee identifies, curates and develops resources for the NSGC community to assess the practice of genetic counseling and to conduct research that informs this practice.
The 2025 RQO Committee charges include:
- Administer NSGC-funded Research Initiative projects
- With guidance from the Board, and in consultation with relevant NSGC groups, staff and consultants, identify a key research question supporting NSGC's Strategic Plan and issue an RFP for the third year of Research Initiative funding
- Conduct the application, review and funding process for specialty or topic-specific proposals submitted by SIGs
Committee Leadership
Chair: Miranda Hallquist
Vice Chair: Laura Amendola
Board Liaison: Shannon Kieran
NSGC Research Initiative
The Research Initiative is a $30,000 NSGC Research Grant meant to foster research that advances the genetic counseling profession. Each year, the NSGC issues a request for proposals on a topic that supports NSGC’s Strategic Initiative. The 2026 Research Initiative topic will be announced at the 2025 NSGC Annual Conference in November. Applications will open in early December.
NSGC is pleased to announce the request for proposals (RFP) for the 2026 Research Initiative: "Investigating and evaluating the use of Artificial Intelligence in genetic counseling practice.” The 2026 Research Initiative aims to evaluate the impact of generative artificial intelligence (AI) technologies on genetic counseling practice, including their potential impact on patient care, professional roles, and ethical standards. Funding in the amount of up to $30,000 is available for a 12-month period. Proposals are due March 1, 2026.
Both new and experienced genetic counselors are encouraged to apply! The principal investigator (PI) or co-investigator must be a genetic counselor and NSGC member.
Please view the full Research Initiative Request for Proposals and submit your proposal here.
If you have any questions, please contact Laura Amendola and Juliet Sullivan.
Past NSGC Research Initiatives:
2024: The 2024 Research Initiative was awarded to Blair Stevens and her research team at the University of Texas Health Science Center at Houston (UTHealth). Her project, “Assessing patient and provider communication surrounding abortion in reproductive genetic counseling” explores how restrictive abortion policies impact the patient-provider experience in reproductive genetic counseling. Findings will be presented at the 2026 Annual Conference.
2025: The 2025 Research Initiative was awarded to Caitlin Mauer Hall and her research team at the University of Texas Southwestern Medical Center in Dallas, Texas. Her project, “Evaluating the Financial Impact and Cost-Effectiveness of Genetic Counselors” compares the cost, revenue, and financial savings of genetic testing services when delivered by genetic counselors versus cardiovascular physicians for patients meeting cardiovascular genetic testing guidelines. Findings will be presented at the 2027 Annual Conference.
Past Committee Projects
Landscape of Quality Measures Related to Genetic Counseling
This list of measures is a result of a collaborative effort by the National Society of Genetic Counselors’ Research Quality and Outcomes Committee and Discern Health, a value-based healthcare policy consulting firm. The first tab includes a scan of existing quality measures, the source, type of measure (Outcome, Structure, Process), clinical area, where the measure maps to the genetic counseling care continuum, steward of the measure, data source and endorsement status. The second tab, labeled “PROMs” is a list of patient-reported outcome measures with a link to the source.
These lists are not meant to be exhaustive, and will evolve over time. Please consider this a starting place as you consider measures for use in genetic counseling quality improvement or outcomes research. A citation will be added if the manuscript is accepted for publication.
To access this list, click here.
For more information, contact Emily Higgs (emily.higgs@ucsf.edu).
Research Infrastructure Development
The RQO Committee is committed to addressing the NSGC memberships’ research needs and supporting NSGC’s research strategy that focuses on the quality of genetic counseling services and outcomes of genetic counseling interventions. To this end, the Committee will develop improved infrastructure, including a NSGC Research Initiative. Ongoing Committee efforts will inform this infrastructure, such as the 2020 Genetic Counseling Quality Landscape Assessment recommendations (described below).
In developing an NSGC research infrastructure, it is important to harmonize research, clinical needs, and resources. While some quality or patient outcome measures may be suitable for both clinical and research settings, some measures primarily fit into one setting. Improving research networking and collaborative opportunities will allow for larger studies across settings and the use of consistent, informative data to increase the power and informative nature of NSGC’s research efforts.
Genetic Counseling Quality Landscape Assessment
In 2020, the NSGC contracted with Discern Health, a healthcare consulting firm, to perform a landscape assessment of the genetic counseling profession and quality measures to help establish a roadmap for NSGC’s research and measure-development efforts. This collaboration identified evidence-based measurement opportunities applicable to genetic counseling models across settings and specialties, helped clarify opportunities and gaps in quality and outcome measurements, and informed pathways to demonstrate genetic counseling value. This work provided a strategic roadmap to prioritize measure development and identified new opportunities to engage in quality-improvement programs.
Genetic Counseling Literature Repository
The RQO committee is pleased to share the digital Genetic Counseling Literature Repository (GCLR), a searchable, PMID-linked, database completely within NSGC’s website. The NSGC GCLR is a resource to identify articles that: 1) document the value and quality of genetic counseling services and 2) describe clinical and research outcomes relevant to genetic counseling patients. This resource includes peer-reviewed scientific literature and select editorials identified via a structured search protocol, conducted monthly by members of the RQO Committee. The design of the repository will facilitate user queries based on annotations determined by the GCLR Subcommittee. The GCLR supports the NSGC Research Initiative and is available to the NSGC membership.
For additional information on the GCLR, please view the video below:
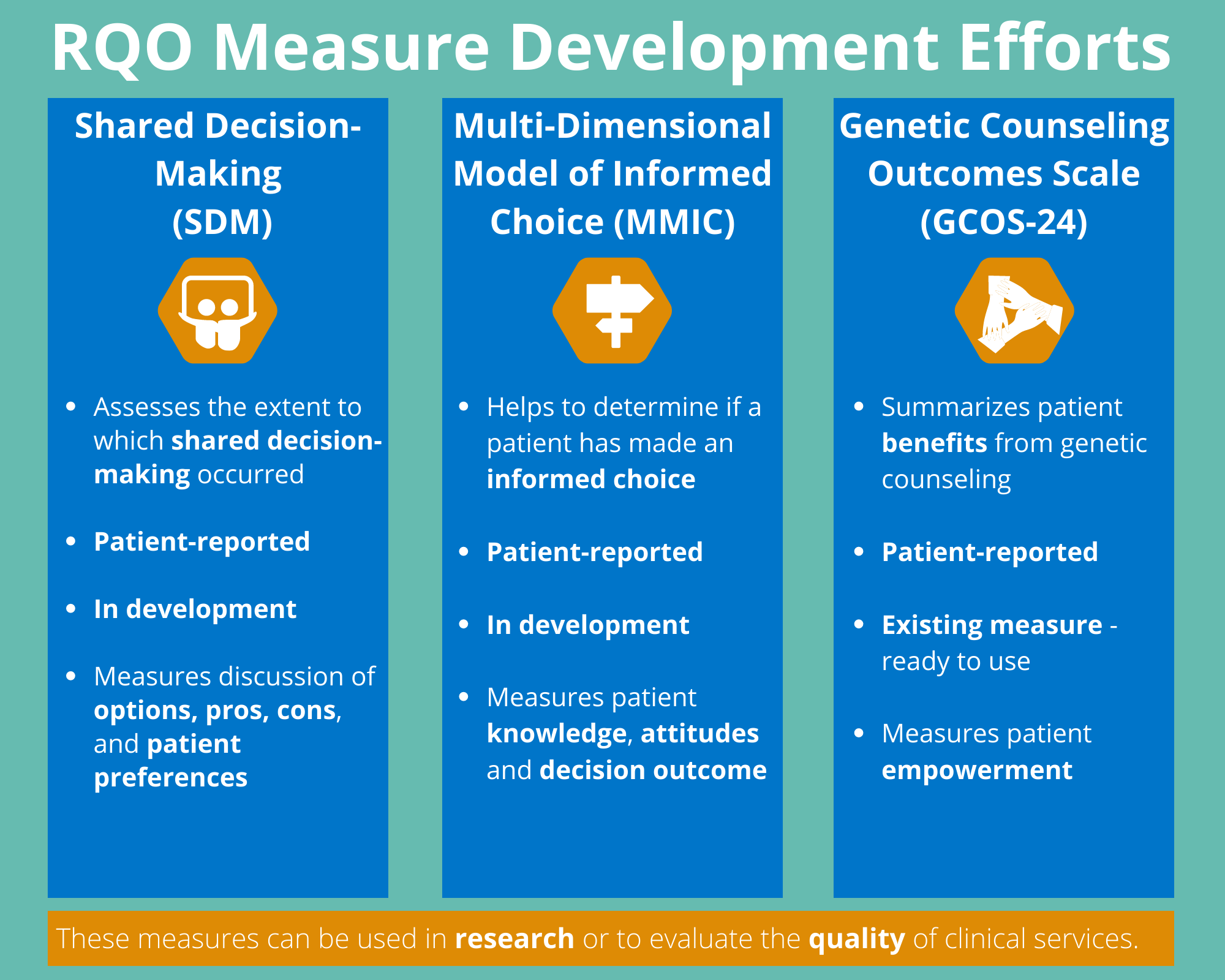
Instrument Measures Development Efforts
The NSGC RQO Committee is charged with exploring measures that will assess patient-reported and research outcomes of genetic counseling and exploring options for formal endorsement of high-quality measures. The development of these measures has typically started in research environments with subsequent adoption into clinical practice. Measures are needed for both purposes and can, at times, be used in both research and clinical settings. The Committee has selected the following measures to further develop because they have already been utilized in research and have high potential as PROMs in clinical settings.
Current Committee efforts currently focus on the following measures (described in more detail in the section below):
- Shared Decision-Making (SDM)
- The Multi-Dimensional Model of Informed Choice (MMIC)
Research Resources
A research question determines the outcomes of a study. If the question focuses on whether participants valued the care that they received, researchers would use a quality PROM as the outcome. If the researcher is conducting a study on genetic counseling service delivery or the type of genomic information returned, the outcome will likely relate to understanding (knowledge), psychological well-being (such as, test-related distress or decisional regret), or clinical outcomes (such as uptake of recommended healthcare or notification of relatives of hereditary risk). The RQO committee has compiled several resources that may be helpful for conducting outcomes-related research. Additional resources can be found in the Research SIG members community.
Definitions used in Patient-Outcomes Measurement
Glossary of key definitions, organizations and programs related to patient outcomes measurement
|
DEFINITIONS RELATED TO QUALITY
|
|
Term
|
Definition
|
|
Quality
|
The safety, timeliness, effectiveness, efficiency, equity, and/or patient-centeredness of healthcare.
|
|
Quality measure
|
Tools that quantify the ability of a healthcare service or healthcare professional to deliver high-quality care in the domains above.
|
|
Outcomes measure
|
Assessment of the impact of the health care service or intervention on the health status of patients
|
|
Patient-reported outcome (PRO)
|
Information collected directly from a patient, their family, caregiver or any consumer related to their health status or experience with healthcare. This may include a report of health-related quality of life, symptoms, experience with a healthcare interaction or a health behavior (eg. smoking).
|
|
Patient-reported outcome measure (PROM)
|
Tool, scale or instrument used to assess patient reported outcomes (PROs). In genetic counseling, examples include the Genetic Counseling Outcome Scale, designed to measure empowerment (McAllister et al., 2011b), and the Perceived Personal Control questionnaire (Berkenstadt et al., 1999). PROMs can be administered before and after use of the service, enabling change-over-time to be measured.
|
|
Patient-Reported Experience Measure (PREM)
|
A subset of PROMs that measure patient satisfaction with a healthcare service (Weldring & Smith, 2013). In genetic counseling, examples include the Genetic Counseling Satisfaction Scale (Tercyak, et al., 2001) and the satisfaction scale developed by Zellerino, et al (2009). PREMs provide important insights into the patient experience of healthcare, but they do not give an indication of improvement in outcomes, as they are only administered after the service has been provided.
|
|
Patient-reported outcome performance measure (PRO-PM)
|
Quantification of quality that is based on aggregated data collected by a patient reported outcome measure (PROM) for use by an entity who is responsible for the quality of care or services delivered, such as a hospital or healthcare practice. They are used for the purpose of performance evaluation and accountability on an institutional and systemic level, or comparing the performance of different healthcare organizations.
|
|
Value
|
The quality of care considering cost that leads to improved patient outcomes. High value care maximizing health outcomes relative to the cost input.
|
|
U.S-BASED ORGANIZATIONS INVOLVED IN QUALITY IMPROVEMENT AND/OR MEASUREMENT
|
|
National Quality Forum (NQF)
|
Organization that endorses PRO-PMs for the purposes of performance improvement and accountability. https://www.qualityforum.org/
|
|
National Committee for Quality Assurance (NCQA)
|
Organization whose goal is to offer ways to measure quality of healthcare plans, medical professionals and practices. They offer accreditation, certification and recognition programs. https://www.ncqa.org/
|
|
PROGRAMS FOR QUALITY MEASUREMENT
|
|
Quality Oncology Practice Initiative (QOPI)
|
A quality program maintained by the (ASCO) that allows users to submit quality data using evidenced-based measures and receive a report with aggregate scores, allowing for benchmarking against other cancer programs. https://practice.asco.org/quality-improvement/quality-programs/quality-oncology-practice-initiative
|
|
|
Merit-based Incentive Payment System (MIPS)
|
A quality program used by the Centers for Medicare & Medicaid Services (CMS) to reward physicians who provide high-quality care with higher reimbursement rates. Performance is measured across several categories focused on quality and cost of patient care, improvements to care processes and use of electronic health records. https://qpp.cms.gov/mips/reporting-options-overview
|
|
|
Alternative payment models (APM):
|
Payment approach used by CMS to reward high-quality care that is provided in a cost-efficient method. https://qpp.cms.gov/apms/overview
|
|
|
Healthcare Effectiveness Data and Information Set (HEDIS)
|
A group of performance improvement tools that encompasses more than 90 measures across 6 domains of care, maintained by the NCQA. https://www.ncqa.org/hedis/
|
|
Key references:
https://www.qualityforum.org/Publications/2012/12/Patient-Reported_Outcomes_in_Performance_Measurement.aspx
https://www.ahrq.gov/talkingquality/measures/six-domains.html
https://health.gov/our-work/national-health-initiatives/health-care-quality/about-health-care-quality
Measures
Shared Decision-Making (SDM)
The SDM measure is intended for patients to complete after a consultation with a healthcare practitioner. This measure has been endorsed by the NQF in several settings already. It is based on a four-item patient-reported survey that assesses the extent to which SDM happens in conversations between patients and healthcare practitioners. The items cover four core behaviors that are necessary for SDM: discussion of options, pros, cons, and patients’ preferences. The survey has been tested extensively in common medical decisions including cancer screening tests, medication decision-making, and surgical decision-making. There is strong evidence of reliability and validity, and differences of 0.3SD-0.5SD have been seen between sites that do vs. do not make an effort to implement SDM (i.e. through decision aids or coaching). More information on the SDM measure is available at: https://mghdecisionsciences.org/about-us/shared-decision-making/
Although there are many genetic counseling ‘decisions’ that could be studied, the Subcommittee is piloting a project through the Massachusetts General Hospital Cancer Center to study SDM in the context of the decision to proceed with hereditary cancer genetic testing. After the pilot phase, the Subcommittee plans to test the measure in other (e.g. prenatal, cardiogenetics) clinical settings.
For more information, contact Kristen Shannon (keshannon@mgh.harvard.edu).
The Multi-Dimensional Model of Informed Choice (MMIC)
NSGC defines genetic counseling as a process of helping individuals understand and adapt to the medical, psychological, and familial implications of genetic contributions to disease. This process includes helping individuals make an informed choice. Yet, it is challenging to know when patients have made an informed choice, which is the outcome of a well-considered decision.
A self-report assessment would be subjective and likely to have a positive bias, as a person intends and hopes that he/she made an informed choice. An objective assessment that includes mastery of information that the decision maker (and practitioners) deems important and determines whether the decision is congruent with one’s values and beliefs is necessary (Marteau, et al., 2001).
The MMIC assesses the relationship among three constructs: relevant knowledge, attitudes toward the decision target, and the decision outcome. Respondents with sufficient relevant knowledge who make a decision in accordance with their attitudes (determined by values and beliefs) have thus made informed choices.
While developed as a research outcome of studies to enhance informed choice, the MMIC is likely to be a valid clinical-services outcome. The MMIC may also offer practitioner-level outcomes data to demonstrate genetic counselors' role in helping patients arrive at informed choices. The MMIC subgroup has prioritized prenatal (NIPT) decisions and cancer-testing decisions as areas to pilot the scale as a clinical outcome of genetic counseling. The RQO Committee will validate these scales in English and Spanish.
Multi-Dimensional Model of Informed Choice (MMIC) References
For more information, contact Susan Christian (Susan.Christian@albertapubliclabs.ca).
Genetic Counseling Outcomes Scale (GCOS)
The Genetic Counseling Outcome Scale (GCOS-24) is a PROM that captures empowerment, a construct summarizing how the patient benefits from genetic counseling (McAllister, et al., 2011). The GCOS-24 has good psychometric properties, with established reliability, internal consistency, responsiveness, and construct validity with no floor or ceiling effects observed (McAllister, et al., 2011). Read more about the GCOS-24 here.
Genetic Counseling Outcomes Scale (GCOS) References
For more information, contact Marion McAllister (McAllisterMF@cardiff.ac.uk).
Grant Writing Resources
At the 2020 and 2021 NSGC Annual Conferences, a Grant Writing Short Course was offered. Below are links to the 15-minute didactic lectures from these sessions, which include how to write specific aims, a research plan, and a budget. There is also a mock grant review session to illustrate how a grant is assessed.
We encourage individuals in the process of writing a funding application or aspiring to write one to explore the other grant writing resources including:
Justice, Equity, Diversity, and Inclusion in Research (J.E.D.I) Resources
The RQO committee is compiling resources that may help clinicians and researchers to collect data and clinical metrics to facilitate research and quality improvement efforts with diverse populations. We will continue to add to this list. Please email Juliet Sullivan (jsullivan@nsgc.org) with suggestions for additional content.
Research SIG Resources
The Research SIG developed this educational resource and has given permission to share this resource with the NSGC membership broadly. The purpose of this document is to provide genetic counselors direction in developing their research skills, particularly in regards to data analysis. In this document you will find links to websites, videos, articles, and other documents submitted by NSGC members for this tool.
Disclaimer: Please note that these resources were compiled by volunteers and were not created by NSGC. Sharing these resources does not constitute endorsement of the information provided. The resources have not been fully vetted for content.
Webinars
July 2022 Demystifying the Research Process: The Research You Are Already Doing Webinar Recording
The first in the series of Demystifying the Research Process. The Research You Are Already Doing webinar includes a conversation with genetic counselors who have collaborated to turn novel clinical experiences into a case series.
January 2022 Research Curious? Tips and Tricks to Publish Your Student Project & other unpublished data Webinar Recording
The final presentation in the Research Curious webinar series closes with Kennedy Borle, Eugene Wong, Christy Smith sharing their experiences of publishing their student research projects after graduation, while balancing the challenges of a new job. This webinar aims to provide guidance for the many others who are navigating publication of their student research and other unpublished data.
September 2021 Research Curious? Tips and Strategies for Conducting a Research Study Webinar Recording
This webinar features genetic counselor, Colleen Caleshu, from GeneMatters. She discusses her successes and lessons learned as she implemented her JEMF-funded research project. The second half of the webinar is a discussion about study implementation, including navigating recruitment and enrollment, deviation from the study design, and other unanticipated challenges.
June 2021 Research Curious? Research Design and Implementation: A Case Presentation and Discussion Webinar Recording
Research Curious webinar series continues with Rebecca Smith, from Geisinger’s Autism & Developmental Medicine Institute. She shares her research story with a focus on how she located the resources and expertise she needed, and the pivots she made, to begin to develop her own project. The second half of the webinar is an open discussion about research-design needs, resources, and participants’ own experiences.
January 2021 Research Curious? Webinar Recording
This webinar explores how genetic counselors go from research-curious to research-involved. RQO Committee members, Karen Wain, Julia Wynn, and Kristen Shannon, will explore how genetic counselors turned their research wonder into research projects. Some of the current and future RQO Committee resources intended to aid genetic counselors in their research journey are also discussed.
January 2021 Webinar Testimonial Video
This quick fun video shares clips from genetic counselors sharing their experience of how they became involved in research.
- 2020 Grant Writing Short Course
- 2021 Grant Writing Short Course
- NSGC Mentors for Research & Grants (https://communities.nsgc.org/network/findmentor),
- JEMF Grant writing resources (https://www.nsgc.org/JEMF)
- NIH grant writing resources including sample applications (https://www.niaid.nih.gov/grants-contracts/sample-applications)